Intro
Why are skin layers important? Well, some tips around our biggest organ functions and structure may come with the secret ‘ingredient’ for your skincare routine. Sounds a little bit nerdy, right? No worries, this article is meant to summarize a very complex topic, so going through it is no easy task.
In any case, you will find some self-explanatory colored images, which will illustrate the key factors for skincare. Additionally, you will find subheadings, highlighting the main idea from each paragraph.
Skin Layers
Skin is the largest organ that we have, also our epithelial tissue. Together with hair and nails represents the integumentary system. Surrounds and protects the organism against outside infections, allergens, and extreme temperatures. Above all, it minimizes water loss from the body creating a balance of fluids and makes possible the synthesis of vitamin D.
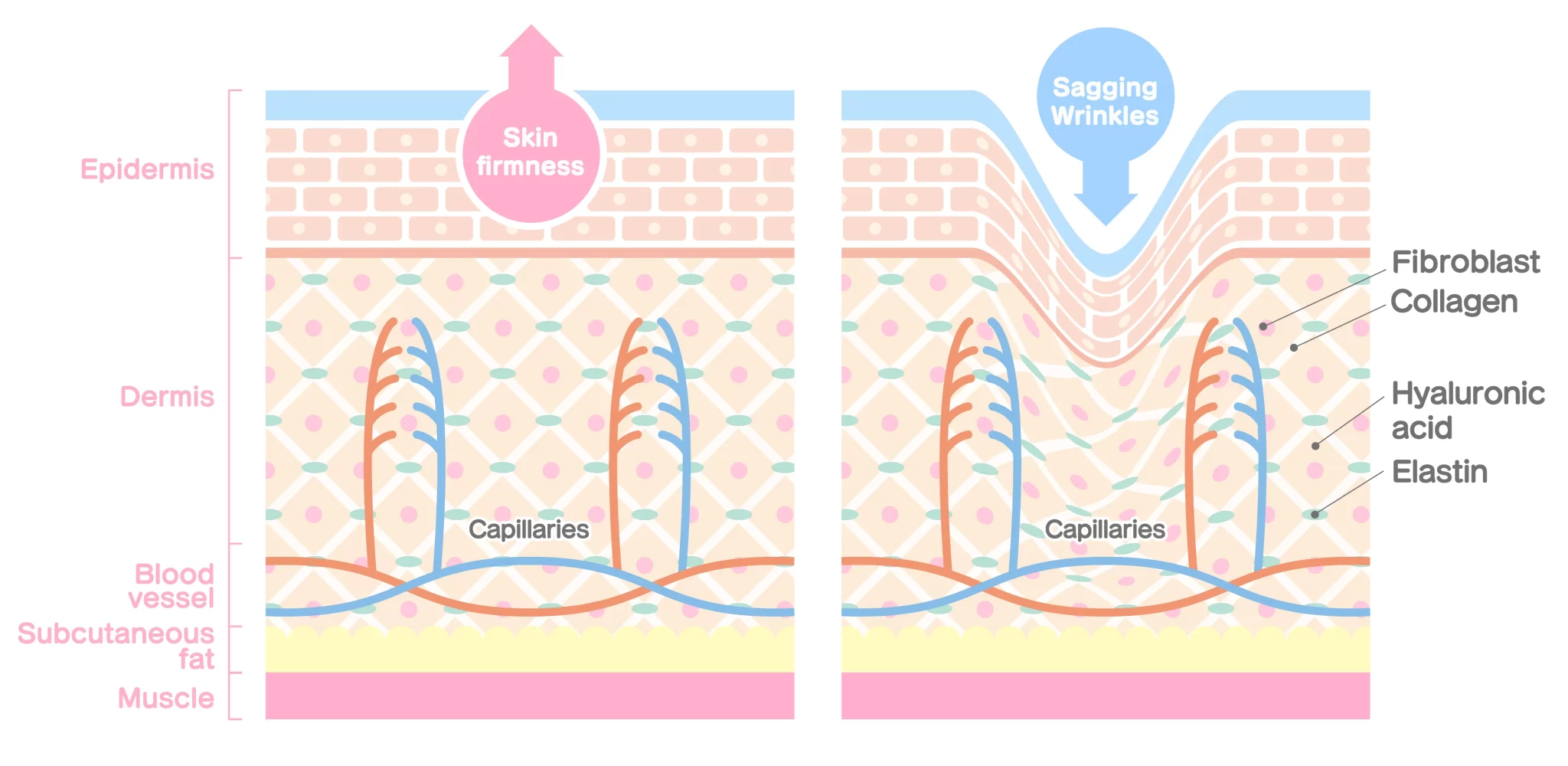
Skin layers and a part of the muscle tissue
Function
Represents our main barrier having multiple adaptive functions, protecting us from the oxidative stress of UV light, being the first defense against infections, allergens and provides adaptive immunological barriers. In addition, it regulates the body water loss into the atmosphere, commonly known as transepidermal water loss, referring to the skin’s ability to retain moisture. The first layer of skin it’s a stratified formation, always under a constant cycle of cell renewal from the basal layer, as we shall see later. It is not vascularized, therefore using oxygen and nutrients that it needs from beneath, rising from Dermis, the second layer of skin. Meaning that your body maintains and produces most of that glowing skin, through a healthy diet. Consume all types of foods, especially proteins, vitamins, and antioxidants.
Cellular constituents
For those interested, the cellular constituents of the epidermis will be listed, such as keratinocytes, melanocytes, immune system cells – Langerhans cells (dendritic cells), and Merkel cells.
Composition
Our dermis is a fibrous layer, full of collagen, elastic fibers, and watery gel-like substances, hosting nerve fibers to record sensations such as temperature, pressure, and pain. However, in the structural composition, we find three types of cells – fibroblasts, macrophages, and mast cells. Also, we have capillaries, blood vessels, hair follicles, sweat glands, apocrine glands, and sebaceous glands (oil ).
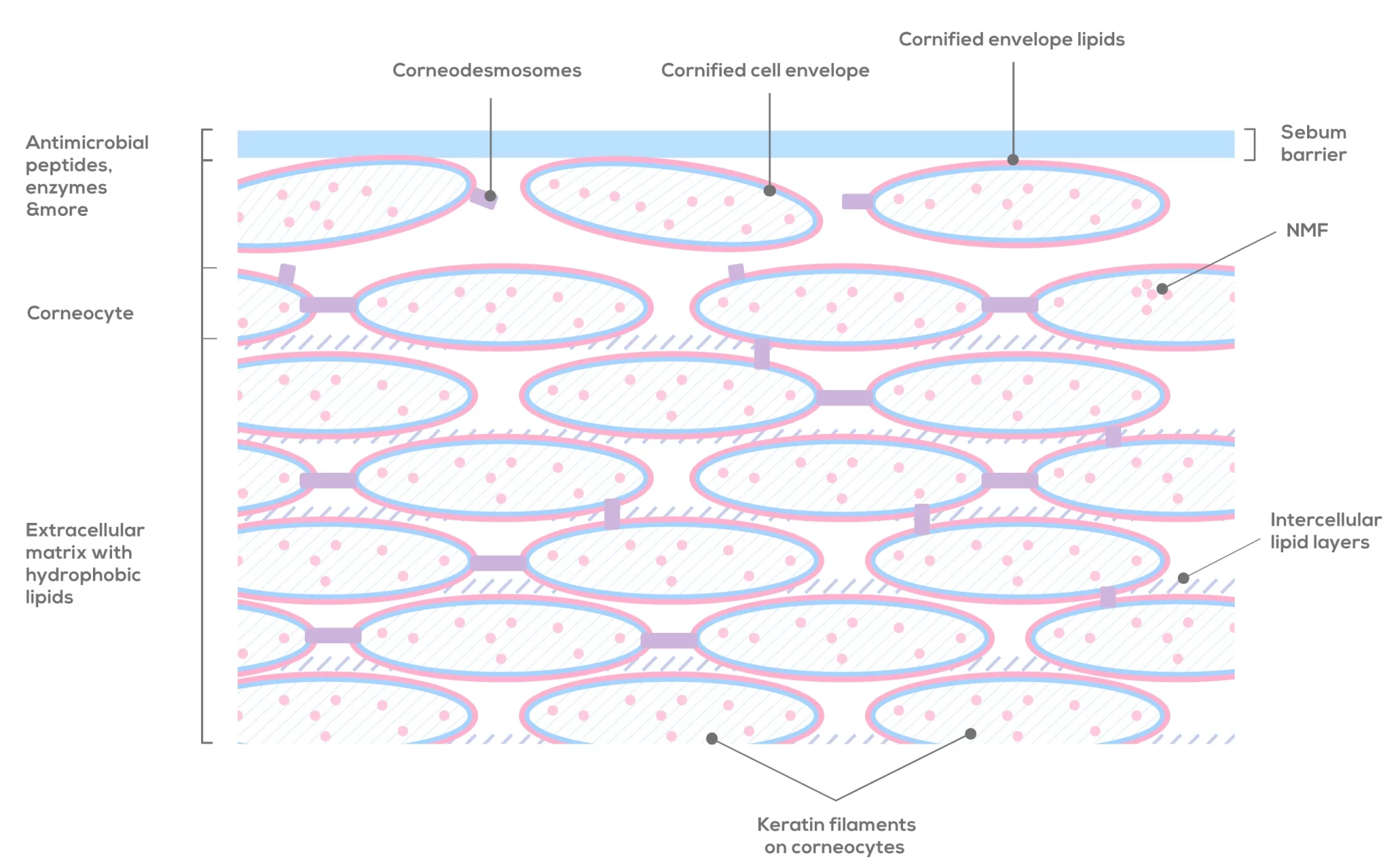
Sebum barrier
Sebaceous glands have small ducts, which lead our healthy oily substance (sebum) to the surface of the skin, up to the stratum corneum. Sebum is our natural protective moisturizer, helping to waterproof the skin, which also makes it harder for hydrophilic molecules to penetrate our skin, through the first layer. Some of its constituents are fatty acid esters like triglycerides, wax esters, squalene, free fatty acids, and unsaturated fatty acids.
As biology taught us, we know it is our adipose connective tissue, often referred to as subcutaneous tissue.
Even more, it produces fat cells, named adipocytes, and has nerves and blood vessels too. Provides insulation, stores energy, absorbs shock, and helps anchor the skin on the muscles.
Stratum corneum layer
Layers of Epidermis
Function
Being the first layer of skin comes with a vital role in protecting the body. Therefore it forms both a physical and antimicrobial barrier, taking charge of skin’s water loss regulation, along with environmental invasions, including even the damaging effects from the ultraviolet radiations.
Composition
Firstly, we need to know that in the stratum corneum we find its extracellular matrix, which is full of lipids arrangements, under the name of lamellar bilayers, or lamellar lipid layers. At the same time, its structural compositions show enzymes, antimicrobial peptides, proteins, acids, and macrophages.
Secondly, in this layer, we have a 20-30 sheet formation of protein-enriched cells, referred to as corneocytes. Inside each corneocyte, we find keratin filaments, along with small molecules called natural moisturizing factors (NMF). As for the outside, each corneocyte is surrounded by a protein layer network, forming the cornified cell envelope, covalently bound with lipids like ceramide. Similar to the previous one, a fresh lipid envelope formation is framing the proteic one.
Each corneocyte holds on to each other through corneodesmosomes, an intercellular adhesion.
Back to the extracellular matrix, which fills the spaces between the cells, we now know it is richer in non-polar lipids (fatty molecules), arranged as lamellar lipid layers. The molecules deriving from lamellar bodies are enzymatically changed into ceramide, cholesterol, and fatty acids, forming a hydrophobic matrix.
From keratinocytes to corneocytes
Meanwhile, in the depths of the basal layer, keratinocyte cells undergo their generation cycle, in order to leave across all other layers up to the skin’s surface, reaching maturity along the way. Keratin and other elements within a keratinocyte degrade its cellular composition throughout the “journey”, ultimately reaching the stratum corneum. As a result, it becomes a corneocyte, now providing mechanical strength for this layer. To sum up, here the final differentiation process takes place, leading to the death of this fibrous cell (corneocyte). Inevitably and necessarily, its final fate is desquamation, our own natural skin peeling.
Skin’s health indicators
Most importantly, this layer is a protective barrier conferring water permeability, and the removal of a thick layer does not always benefit the skin.
From the skin surface, water evaporates and is absorbed too daily and we measure it under all standard conditions to determine transepidermal water loss (TEWL) quantity, indicating our natural hydration or a potential disorder in the protective barrier.
Just as we learned, cells migrate from underneath so we will find living keratinocytes in here as well. After that, cells changed into more granular cells, full of keratohyalin protein. For this protein composition, we will name keratin and profilaggrin. Keratinocytes eventually infiltrate the stratum corneum within other reactions, and release the lamellar bodies, with proteins and lipids. Among other structural modifications is filaggrin, which undergoes cell degradation until they become free amino acids and other derivatives, commonly named natural moisturizing factors (NMF).
The keratinization has its beginnings in this layer, meaning that the formation of the keratin barrier begins. Note that keratin and filaggrin, along with other proteins, form tonofibrils (keratin intermediate filaments), which in turn create adhesion between them through desmosomes. Due to this, our skin gains strength and flexibility.
Described as the regenerating area, the stratum basale is a place for cell division, under the name of mitosis. That is to say, here all new cell production happens, often comparing this layer to a cell factory, a process performed continuously by basal keratinocyte stem cells. Newly formed cells go to the surface through each layer, growing, dividing, evolving, and in the end, being released into the atmosphere. We exfoliate them from the surface of the skin, to trigger more often mitosis, the formation of new cells.
To cut a long story short, it is the main source of keratinocytes, melanocytes (melanin-producing cells), and Merkel cells.
Conclusion
In conclusion, this article is intended to provide you with basic knowledge about our skin and to strengthen your experience for the posts that follow, dedicated entirely to skin care and skin science.
Article resources
- Lumen learning – Courses. Biology for Majors II. Module 24: The Integumentary System. Hypodermis.
- Steven AC, Steinert PM. J Cell Sci. 1994 Feb. “Protein composition of cornified cell envelopes of epidermal keratinocytes”. 107 ( Pt 2):693-700. PMID: 8207091.
- Aileen Sandilands, Calum Sutherland, Alan D. Irvine, and W. H. Irwin McLean. “Filaggrin in the frontline: role in skin barrier function and disease”. J Cell Sci. 2009 May 1; 122(9): 1285–1294. Published online 2009 Apr 22. doi: 10.1242/JCS.033969. PMID: 19386895.
- Karen L. Campbell DVM, MS, DACVIM, DACVD, Carol A. Lichtensteiger DVM, PhD, DACVP, in Small Animal Dermatology Secrets, 2004. “STRUCTURE AND FUNCTION OF THE SKIN”. doi.org/10.1016/B978-1-56053-626-0.50005-7.
- Golara Honari, Howard Maibach, in Applied Dermatotoxicology, 2014. “Chapter 1 – Skin Structure and Function”. doi.org/10.1016/B978-0-12-420130-9.00001-3
- Ehrhardt Proksch, Johanna M. Brandner, Jens‐Michael Jensen. Accepted for publication 1 July 2008. “The skin: an indispensable barrier”. PDF. doi.org/10.1111/j.1600-0625.2008.00786.x.
- Dr. Anthony Yung, Dermatologist, Waikato District Health Board, Hamilton, New Zealand. 2007. “Structure of normal skin”.
- By Yolanda Smith, B.Pharm. Reviewed by Dr. Liji Thomas, MD. “What is the Dermis?”
featured image & image 1. source: shutterstock.com